What is cervical cancer?
Cervical Cancer is a cancer which develops in the neck of the womb. Although it is the tenth most common cancer in Singaporean women, its prevalence has steadily declined over the past 50 years because it is highly preventable and treatable, especially when picked up early.
What are the signs and symptoms of cervical cancer?
Early cervical cancer is typically asymptomatic (no signs and symptoms) and this leaves many women unaware of its presence until the later stages. Thus, regular cervical cancer screening is essential.
Common symptoms of cervical cancer:
- Irregular or heavy vaginal bleeding (between menses or after menopause)
- Pain during sexual intercourse or bleeding after intercourse
- Abnormal vaginal discharge
- Pelvic or lower back pain
What are the cervical cancer risk factors?
The most important risk factor for cervical cancer is Human Papillomavirus (HPV). HPV spreads from person to person during skin-to-skin contact. It is the most common sexually transmitted virus. It is responsible for 99% of cervical cancers. Having persistent HPV infection poses a major risk for cervical cancer. Fortunately, HPV vaccinations are now widely available.
Other risk factors include:
- Cigarette smoking
- Oral contraceptive use for more than 5 years
- Factors predisposing to HPV infections, such as multiple sexual partners
How can I prevent cervical cancer?
HPV vaccination greatly reduces the likelihood for developing cervical cancer. It is safe and effective and readily available in Singapore.
Other preventive measures include:
- Screening regularly for cervical cancer with PAP test and HPV test
- Practicing safe sex by using condoms
- Limiting the number of sexual partners
- Avoiding sexual intercourse with people who have had many partners
- Avoiding sexual intervourse with people who are infected with genital warts
- Not smoking
More about HPV and the cervical cancer vaccine
HPV vaccines have been proven to be effective in preventing cervical cancer and the pre-cancer, Cervical Intraepithelial Neoplasia (CIN).
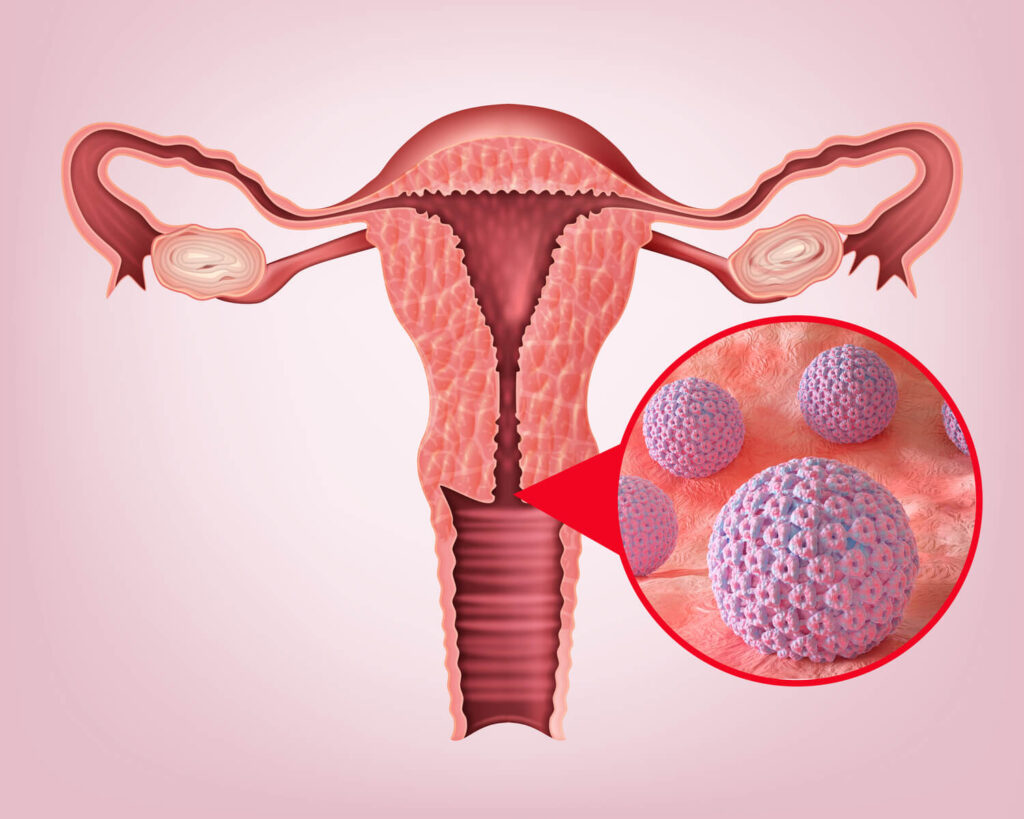
Human papillomavirus in cervix
There are more than 150 types or “strains” of HPV. Most HPV infections do not cause any health problems. Some types of HPV cause warts. These warts can grow anywhere on the body and are often found on the hands and feet. They are contagious and spread by touch, but they do not cause cancer. About 40 types of HPV are called “genital HPV.” Genital HPV spreads by skin contact, usually during vaginal, anal, and oral sex. Some types of genital HPV cause genital warts. They do not lead to cancer. They are known as low-risk HPV. Common types of low-risk HPV include HPV-6 and HPV-11. Other types of genital HPV are known as high-risk HPV. Over time, the infection can turn normal cells into precancer or cancer.
There are 3 HPV vaccines currently available. Gardasil 9 helps prevent infection from 7 high-risk HPV: HPV-16, HPV-18, and 5 other less common types of HPV linked to cancer. The vaccine can also prevent 2 low-risk HPV known to cause 90% of genital warts.
The other 2 vaccines are Gardasil, which helps prevent infection from 2 high-risk HPV and 2 low-risk HPV, while Cervarix helps prevent infection from 2 high-risk HPV.

The vaccine is most effective for women who are not HPV-positive and have never had sex. Those who are already sexually active, have had prior genital warts, abnormal Pap smear or HPV infection can still be vaccinated although it is less helpful. However, the HPV vaccine cannot eliminate any existing HPV infection.
After vaccination, regular screening is still necessary for cervical cancer prevention as there are other cancer-causing subtypes of HPV that are not covered by current vaccines.
Cervical cancer screening to detect cervical cancer early
Although prevention is better than cure, it is still important to screen regularly for cervical cancer. Diagnosing it at an early stage is associated with a good prognosis, with a 5 year survival between 80% to 95%.
There are 2 screening tests for cervical cancer: Pap testing and HPV testing.
- Pap testing is recommended for women who have had sex or are sexually active. These should be done once every three years from the age of 25 years.
- HPV-DNA test has been found to be much more sensitive in detecting cervical cancer and pre-cancers, HPV DNA testing is recommended for women once every 5 years from the age of 30 years.
Cervical cancer diagnosis and treatment
Cervical cancer is typically diagnosed with an abnormal PAP test or HPV DNA test. Confirmatory tests will need to be performed. This includes:
- Colposcopy: A special instrument, the colposcope, helps doctors to visually examine the cervix for any abnormalities, lesions or tumors
- Cervical biopsy: A sample of abnormal tissue is obtained for the cervix, for more definitive examination by microscopy
Your cervical cancer specialist will help determine the most suitable treatment for you. The various treatments include:
- Surgery: The removal of malignant tissues and any surrounding damage
- Radiotherapy: High doses of radiation used to kill cancerous cells and reduce tumour size
- Chemotherapy: Drug treatment to kill rapidly multiplying cancerous cells
- Targeted therapy: Drug treatment given in addition to chemotherapy to improve response to treatment and survival for late-stage cervical cancer
- Immunotherapy: A treatment for late-stage cervical cancer which utilizes the body’s own immune cells to kill cancerous cells
If you are looking for a cervical cancer specialist, you may wish to consult Dr Lynette Ngo.
Dr Lynette Ngo is a highly experienced medical oncologist specializing in women’s cancers. She began her oncology specialization in 2005 at the National Cancer Centre and is now part of the professional team of oncologists at Curie Oncology.